How do geographic healthcare workforce trends shape the future of patient care across urban and rural America? The U.S. healthcare system faces significant challenges related to the geographic distribution of healthcare professionals. Urban areas often boast abundant healthcare providers, while rural and underserved regions struggle with shortages. This imbalance affects millions of people’s access to healthcare, outcomes, and quality of life. This article explores workforce trends, delves into the disparities between urban and rural locations, and highlights potential solutions to bridge these gaps.
Understanding the Geographic Distribution of Healthcare Professionals
Why Geographic Distribution Matters
The location of healthcare professionals plays a crucial role in the accessibility and quality of care. Urban centers often attract specialists, leading to better outcomes, while rural and underserved regions face barriers such as:
- Long travel distances for patients.
- Delays in receiving timely medical care.
- Increased health risks due to inadequate resources.
According to the Health Resources and Services Administration (HRSA), approximately 30% of Americans live in Health Professional Shortage Areas (HPSAs), underscoring the urgency of addressing this issue.
Trends in Healthcare Workforce Distribution
Urban vs. Rural Divide
Urban areas benefit from higher concentrations of healthcare professionals due to better infrastructure, opportunities for professional growth, and lifestyle preferences. Examples include:
- Washington D.C.: 65.8 physicians per 10,000 residents.
- Massachusetts: 44.2 physicians per 10,000 residents.
In contrast, rural states like Idaho and Mississippi average fewer than 20 physicians per 10,000 residents, contributing to care disparities.
Specialty Distribution
Specialists such as cardiologists and oncologists are more likely to practice in urban areas, while generalists and primary care providers are more evenly distributed. However, the shortage of primary care physicians in rural regions remains a significant concern.
Growth in Allied Health Professions
Allied health professionals, including physical therapists and pharmacists, play a vital role in bridging gaps. However, projections also indicate shortages in these fields, potentially exacerbating challenges.
Challenges Affecting Healthcare Workforce Distribution
Incentives and Financial Barriers
- Urban centers offer higher salaries and better job stability.
- Rural areas face financial constraints, limiting their ability to attract talent.
Infrastructure Limitations
- The lack of state-of-the-art facilities in rural areas deters healthcare professionals.
- Limited access to continuing education and professional development hinders growth.
Lifestyle Preferences
- Younger professionals often prioritize urban living for cultural, social, and career-related reasons, leaving rural areas understaffed.
Solutions to Bridge the Gap
Telemedicine
Telemedicine has become a powerful tool for extending healthcare services to underserved areas. By leveraging technology, patients in rural regions can access specialists without traveling long distances.
Discover strategies to enhance your career through telemedicine connections.
Incentive Programs
Government and private organizations are implementing programs such as:
- Loan forgiveness for professionals working in HPSAs.
- Grants to improve rural healthcare infrastructure.
- Tax incentives for providers in underserved areas.
Workforce Training and Development
Investing in training programs tailored to rural healthcare needs can prepare professionals to address unique challenges. Additionally, partnerships between urban hospitals and rural clinics can promote knowledge sharing.
Benefits of Addressing Workforce Disparities
- Improved Patient Outcomes: Timely access to care reduces health complications.
- Economic Growth: Enhanced healthcare infrastructure supports local economies.
- Equity in Care: Equal distribution ensures everyone receives quality healthcare, regardless of location.
Addressing the geographic disparities in healthcare workforce distribution is a shared responsibility. Policymakers, healthcare organizations, and professionals must collaborate to create a more equitable system.
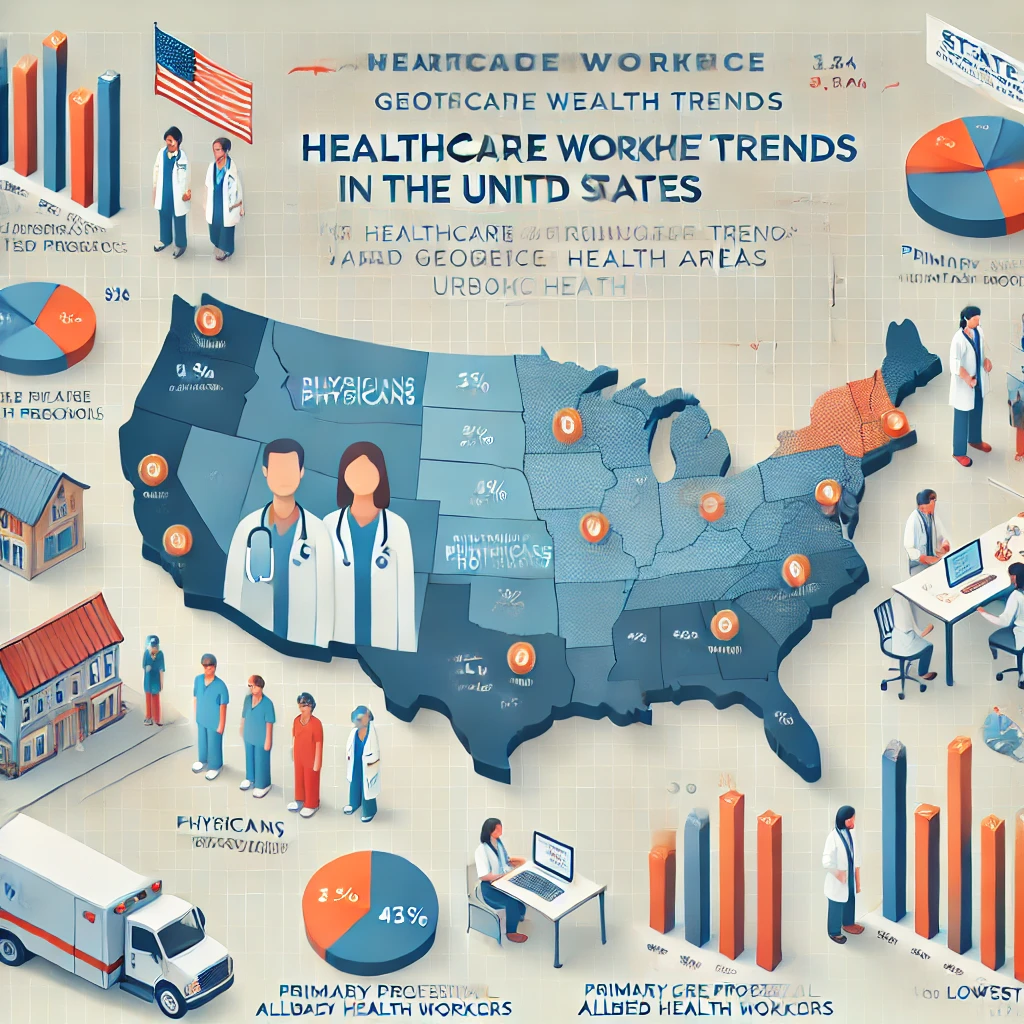
Geographic Healthcare Workforce Trends in the U.S.
| Region/State | Physicians per 10,000 Residents | Primary Care HPSAs | Key Trends |
|---|---|---|---|
| Washington D.C. | 65.8 | Low | Highest physician density; urban-centered healthcare workforce. |
| Massachusetts | 44.2 | Low | Strong presence of specialists and advanced healthcare systems. |
| Idaho | 19.0 | High | Uneven distribution; urban areas are well-served, and rural areas are not. |
| Mississippi | 19.8 | High | High disparities; underserved areas dominate rural regions. |
| Wyoming | 20.2 | High | Sparse population; limited healthcare infrastructure. |
| National Average | 28.2 | Moderate | Uneven distribution: urban areas are well-served, and rural areas are not. |
Key Takeaways:
- Urban regions, like Washington D.C., exhibit dense physician populations, supporting diverse medical needs.
- Rural states like Idaho and Mississippi face severe shortages, creating challenges for equitable healthcare access.
- Understanding these geographic healthcare workforce trends is essential to addressing disparities and improving outcomes nationwide.
Bridging Gaps: Addressing Geographic Healthcare Workforce Trends
Addressing geographic healthcare workforce trends is vital to ensuring equitable care across the U.S. Solutions like telemedicine and workforce incentives can bridge disparities, improve outcomes, and create a more inclusive healthcare system.
FAQs about Geographic healthcare workforce trends
1. What are Health Professional Shortage Areas (HPSAs)?
HPSAs are regions with a significant shortage of primary care, dental, or mental health professionals. They are identified by HRSA and often include rural and underserved urban areas.
2. How can telemedicine help underserved areas?
Telemedicine bridges the gap by connecting patients with healthcare providers through technology, reducing the need for travel and ensuring timely care.
3. What are some incentives for healthcare professionals to work in rural areas?
Incentives include loan forgiveness programs, grants, and tax benefits for professionals serving in designated HPSAs.
4. What is the projected shortage of healthcare professionals in the U.S.?
Up to 139,000 physicians in primary care and rural specialties could be needed in the U.S. by 2030.
5. How can allied health professionals contribute to reducing disparities?
Allied health professionals provide essential support, such as physical therapy and pharmacy services, ensuring holistic care in underserved areas.